Science
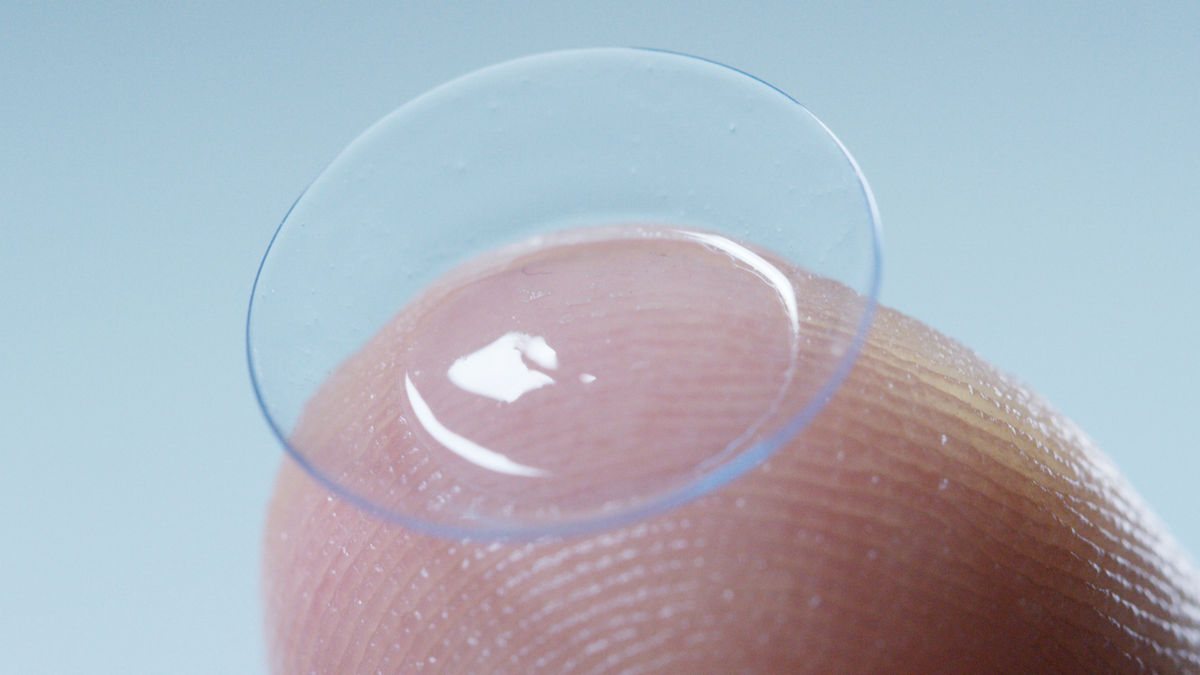
Designing an atropine-eluting contact lens for myopia
In this article:
This study found that while microemulsion-based contact lenses successfully stabilized and released atropine base, providing a potential sustained drug delivery method for myopia control, the formulations were highly cytotoxic to human corneal epithelial cells, highlighting the need for further development to ensure ocular safety before clinical application.
Paper title: Designing a Contact Lens with Atropine Base Using a Microemulsion Technique
Authors: Aziz MA (1), Maulvi F (1), Desai DT (2), Kuppusamy R (1, 3), Mazumder K (1, 4), Hui A (1, 5), Stapleton F (1), Willcox M (1)
- School of Optometry and Vision Science, University of New South Wales, Sydney, NSW, Australia
- Maliba Pharmacy College, Uka Tarsadia University, Surat, India
- School of Chemistry, University of Sydney, Sydney, NSW, Australia
- Department of Pharmacy, Jashore University of Science and Technology, Bangladesh
- Centre for Ocular Research and Education, University of Waterloo, Waterloo, Ontario, Canada
Date: Published online February 9, 2025
Reference: Aziz MA, Maulvi F, Desai DT, Kuppusamy R, Mazumder K, Hui A, Stapleton F, Willcox M. Designing a contact lens with atropine base using a microemulsion technique. Contact Lens Anterior Eye. 2025 Feb 9.
Summary
Atropine eye drops and myopia control contact lenses are widely used to slow myopia progression, and emerging research indicates the benefit of combining atropine with optical treatments. Atropine’s efficacy is limited by rapid ocular clearance, and previous studies have shown that drug-eluting lenses can sustain ocular drug delivery, potentially improving treatment outcomes. However, stabilizing atropine in a contact lens system remains a challenge.
This in-vitro study aimed to develop and evaluate a microemulsion-based atropine delivery system for contact lenses to enhance stability and controlled drug release. Unlike atropine sulfate, which is water-soluble and commonly used in eye drops, atropine base is more lipophilic, potentially improving drug absorption and sustained release when incorporated into contact lenses. The goal was to improve the stability of atropine and enhance its release, addressing the rapid clearance issue seen with atropine eye drops.
- Atropine stability: Atropine base was more stable at pH 6.5, with only 4% degradation over one year at room temperature, compared to 10% degradation at pH 7.4.
- Microemulsion (ME) properties: The formulated microemulsions had small, stable globules (17–21 nm in size), with ME 6.5 showing slightly larger globules than ME 7.4.
- Drug uptake and release: MiSight 1 day contact lenses successfully absorbed atropine base from ME 6.5 (4.25 ± 1.67 µg), with most of the drug (3.52 ± 0.03 µg) released within 2 hours.
- Material characteristics: Loading atropine into MiSight lenses had minimal impact on their equilibrium water content and transparency, maintaining optical clarity in the visible spectrum.
- Cytotoxicity concerns: A significant limitation was observed in the in vitro safety evaluation. Atropine base released from the lenses led to substantial cytotoxic effects on human corneal epithelial cells, reducing cell viability to less than 5% after 24 hours.
Despite demonstrating effective drug release and stability, the study highlights a major challenge in that the atropine base in its current formulation is toxic to corneal cells. Future research is needed to refine the formulation to improve biocompatibility while maintaining therapeutic efficacy.
What does this mean for my practice?
The findings highlight both the promise and the challenges of delivering atropine via contact lenses for myopia control. While this approach aims to provide sustained drug release, improve patient adherence, and reduce systemic side effects compared to atropine eye drops, key limitations must be addressed before clinical application.
- Potential benefits: The study confirms that atropine base can be successfully incorporated into contact lenses while maintaining lens clarity, water content, and comfort-related properties. A sustained-release mechanism could offer better compliance in children, minimizing the peaks and troughs of drug concentration seen with eye drops.
- Dosing implications: The study suggests that contact lenses could achieve effective therapeutic doses comparable to 0.01% atropine eye drops, with potentially improved bioavailability and prolonged ocular surface exposure.
- Critical safety concerns: The major limitation is the significant cytotoxicity observed in human corneal epithelial cells. The microemulsion formulation, rather than atropine itself, is likely responsible, necessitating reformulation to improve biocompatibility.
- Clinical readiness: While the concept of atropine-releasing contact lenses is promising, they are not yet suitable for clinical use due to safety concerns. Future refinements in drug delivery methods and biocompatibility are essential before this technology can be integrated into myopia management.
What do we still need to learn?
While this study demonstrates the feasibility of atropine-releasing contact lenses for myopia control, several critical questions remain before this technology can be applied in clinical practice. The most pressing concern is the cytotoxicity of the atropine-loaded lenses, which significantly reduced human corneal epithelial cell viability. Future research must refine the microemulsion formulation or explore alternative drug delivery systems to ensure ocular safety.
Additionally, this in-vitro study did not assess the long-term effects of sustained atropine release on ocular tissues or myopia progression. The rapid release of atropine within two hours raises concerns about whether the lenses provide prolonged therapeutic benefit throughout the day. More studies are needed to optimize drug retention and release kinetics, and the impact of this on short-term eye health and long-term myopia progression.
Finally, while the study focused on MiSight 1 day lenses, it remains unclear whether these findings would extend to other contact lens materials. Future research should investigate how different lens designs and compositions affect atropine stability, release profiles, and patient tolerability in real-world settings.
Abstract
Purpose: Myopia or near-sightedness is a global vision problem. Atropine eye drops and myopia-controlling contact lenses can help to slow down its progression, but neither is sufficient alone. The present research work was conducted to design a contact lens embedded with an atropine base within a microemulsion system. The goal was to improve the stability of atropine base and facilitate its release from the lens, preventing the rapid clearance observed with atropine eye drops.
Methods: Two microemulsions, one with a pH of 7.4 and the other with a pH of 6.5, were developed using the surfactant D-alpha-tocopherol polyethylene glycol 1000 succinate (TPGS), the co-surfactant polyethylene glycol 400 (PEG 400), the emulsifier Capmul MCM C8, atropine base, and phosphate-buffered saline (PBS). The microemulsions were kept at room temperature (21 °C) and the amount of the atropine base in microemulsions were checked periodically over one year using reverse-phase High Performance Liquid Chromatography (RPHPLC) to determine its stability. The globule size of the formulations was measured using a zetasizer. MiSight contact lenses were soaked in the atropine base microemulsion formulations for 24 h, and the amount of atropine base loaded into contact lenses and released in PBS was measured by a RPHPLC. ISO 10993-5 guidelines were used to measure the in vitro cytotoxicity of atropine base loaded contact lenses.
Results: The atropine base was more stable in the microemulsion at pH 6.5 (ME 6.5) with less than 4 % degradation, compared to a 10 % degradation at pH 7.4 (ME 7.4). The globule sizes of the microemulsions ranged between 17-21 nm. MiSight lenses absorbed4.25 ± 1.67 µg atropine base from ME 6.5, with the majority of the atropine base (3.52 ± 0.03 µg) released within 2 h. However, elutes from atropine base loaded contact lenses were toxic to human corneal epithelial cells (HCECs), reducing cell viability to less than 5 % after 24 h.
Conclusions: While the microemulsions were stable and the contact lenses released sufficient amounts of atropine base, future studies are needed to address the toxicity issue.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.












