Clinical
MiYOSMART in Practice: Expert insights on complex clinical questions
Sponsored by
In this article:
This article explores how HOYA MiYOSMART (DIMS) spectacle lenses are applied in real-world practice, with expert insights on managing complex cases such as pre-myopia, high myopia, astigmatism, anisometropia, binocular vision disorders, and special populations beyond the scope of clinical trials.
Myopia control interventions have undergone rigorous evaluation over the past decades, with evidence drawn from both gold-standard randomized controlled trials (RCTs) and retrospective analyses. While these studies provide a robust foundation for clinical decision-making, not every patient fits neatly into the profile of participants represented in research. In real-world practice, clinicians often face additional complexities—such as high astigmatism, binocular vision disorders, and co-existing health conditions—that require tailored strategies to balance therapeutic efficacy with visual function.
The original Defocus Incorporated Multiple Segments (DIMS) spectacle lens RCT included Chinese children aged 8-13 years with low and moderate myopia between -1.00D and -5.00D, and astigmatism or anisometropia of no more than 1.50DC. They had monocular best corrected visual acuity (VA) of 0.00 logMAR (6/6) or better, normal binocular vision function, and no other significant health conditions.
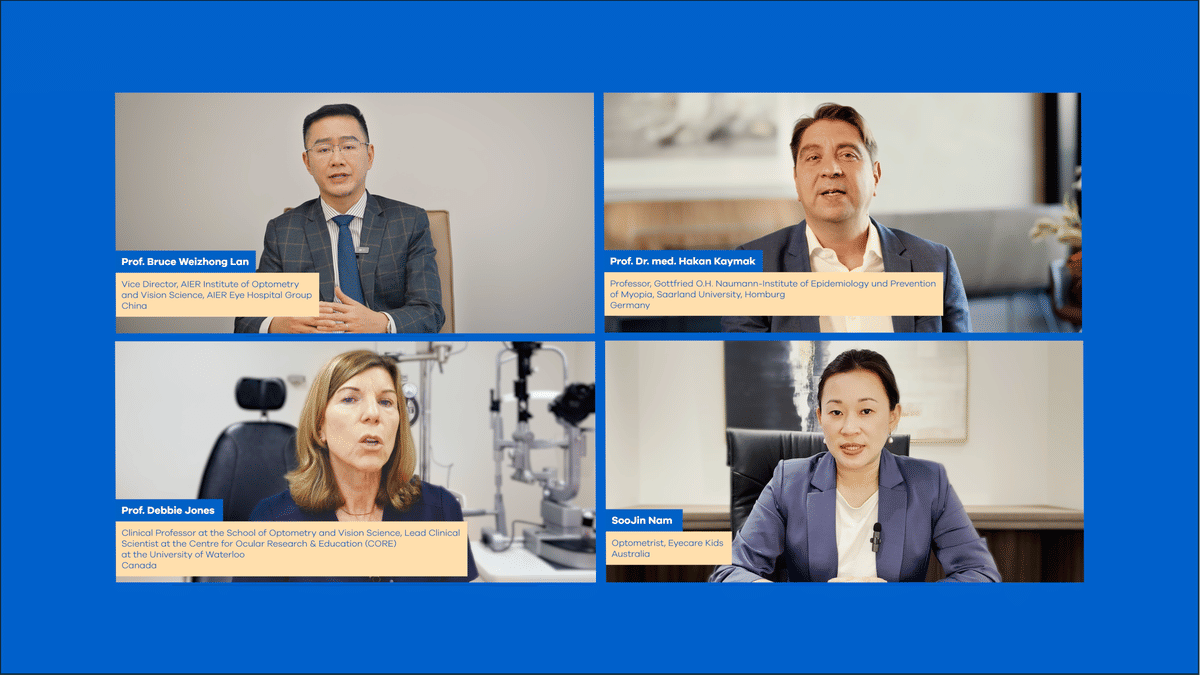
Drawing on content from video interviews conducted with four Key Opinion Leaders (KOLs), which will be made available on HOYA Learning Centre, this article looks at how DIMS spectacle lenses — commercially known as HOYA MiYOSMART — are being used in varied and sometimes complex clinical situations. It covers management approaches for pre-myopia, high myopia, and challenging refractive or functional cases, with key opinion leaders sharing their real-world experiences:
- Prof. Bruce Weizhong Lan, Vice Director of AlER Institute of Optometry and Vision Science, AIER Eye Hospital Group, China
- Prof. Hakan Kaymak, Professor at Gottfried O.H. Naumann-Institute of Epidemiology and Prevention of Myopia, Saarland University, Homburg, Germany
- Prof. Debbie Jones, Clinical Professor at the School of Optometry and Vision Science, and Lead Clinical Scientist at the Centre for Ocular Research & Education (CORE) at the University of Waterloo, Canada
- Ms. SooJin Nam, Optometrist at Eyecare Kids, Sydney, Australia.
Managing Pre-Myopia: Delaying the Onset
Pre-myopic children refer to children who are not yet myopic but are at elevated risk of developing it. Intervention for pre-myopia is gaining traction, as we now know that delaying the onset of myopia can have a greater long-term impact than managing myopia progression after it has already developed. Delaying myopia onset by just one year can reduce the final level of myopia by approximately 0.75D, which is comparable to the effect of 2-3 years of myopia control treatment in already myopic children.
Read more in our article How to identify and manage pre-myopes, which provides a framework for identifying, explaining and managing children at risk, including environmental modifications and treatment with an evidence-based myopia control solution.
Traditionally, interventions for pre-myopia have centred on modifying the visual environment.
- The clinical rationale for delaying onset: Debbie Jones, while cautious due to the current lack of large-scale evidence, supports the rationale for early intervention. She notes that later onset of myopia is associated with a reduced likelihood of developing very high prescriptions in adulthood, reinforcing that delaying onset remains a clinically sound goal—particularly as myopia is now widely recognised as a progressive disease rather than a benign refractive state.
- Proactive prescribing: Bruce Lan explained that some clinicians are now proactively prescribing MiYOSMART spectacle lenses to pre-myopic children. He references animal studies suggesting that projecting myopic defocus on the retina—even before refractive myopia manifests—can slow or delay its onset. While peer-reviewed human data remains limited, anecdotal reports from practitioners in his region have shown promising outcomes.
- Strong family history as a trigger for early action: Hakan Kaymak emphasized that initiating treatment in children with a strong family history of myopia—such as those with myopic parents and siblings—is often well-received by parents. These families are typically more motivated and understand the importance of early action.
A key challenge to also consider when introducing an optical intervention is compliance—because pre-myopic children have no visual symptoms, they may be less inclined to use an intervention that offers no immediate, tangible benefit. DIMS spectacle lenses, however, appear to be well-tolerated in this group, with early efficacy data showing smaller changes in spherical equivalent refraction (SER) and axial length (AL) over 9 months.
High Myopia: Complexity Demands Combination Approaches
Most clinical trials on myopia control have included children with prescriptions up to −6.00D, leaving limited evidence on the effectiveness of interventions for higher myopes.
To address high myopia in children, a multifaceted approach may be required:
- Managing very high prescriptions: Bruce Lan described one case involving a −14.00D prescription. He managed this by prescribing −10.00D* MiYOSMART spectacle lenses and adding −4.00D single vision soft contact lenses to bridge the refractive gap, for simultaneous wear. This approach provided both myopia control and functional daytime vision. While approaches like this will vary based on available prescription ranges for both myopia control spectacles and contact lenses, at Myopia Profile we would tend to recommend correcting as high a prescription as possible with one modality and also considering the important benefits of contact lenses for high myopes. If single vision contact lenses are available in the full prescription, plano or low-powered myopia control spectacles like DIMS spectacle lenses could be considered for the myopia control effect.
- Combination treatment as first-line management: Hakan Kaymak said he routinely initiates combination treatment for children with high myopia, typically prescribing MiYOSMART spectacle lenses in tandem with low-dose atropine (0.05%). In his experience, monotherapy alone tends to yield limited success in these high-risk cases. New research has recently been published on combining 0.025% with MiYOSMART spectacle lenses, showing boosted efficacy over 12 months and good acceptance of treatment.
9 - The importance of frequent monitoring: Soojin Nam explained that her clinic uses a comprehensive protocol for high myopia management, including retinal imaging, Optos Ultra-widefield scans, axial length tracking, topography, and cycloplegic refractions. She allocates 40-minute appointments to these cases, noting that while this is time-intensive, it builds trust and demonstrates value to parents.
Ultimately, managing very high myopia demands flexibility and creativity, combining available treatments in a way that meets both the visual and therapeutic needs of each patient.
Learn more about how to approach these special cases in our articles How should we manage high myopia? and High myopia in childhood - special considerations and safe management.
Refractive Complexity: Astigmatism and Anisometropia
Conditions like astigmatism and anisometropia can add unique challenges to myopia management. This is because these patients may fall outside standard lens parameters and require custom combinations or layered modalities. As for very high myopia, contact lenses may supplement spectacles or vice versa, and alternative strategies may be needed to maintain both efficacy and visual function.
Astigmatism
Astigmatism requires careful correction to avoid undercorrection, which can promote myopia progression.
Spectacle-based myopia control designs, such as MiYOSMART spectacle lenses, can correct more astigmatism than contact lenses typically can, while also slowing myopia progression. However, limitations still exist—MiYOSMART spectacle lenses are only available up to -4.00DC, and their efficacy in very high or irregular astigmatism has not been fully validated, with the initial study including children with up to 1.50DC.1 If astigmatism increases significantly in a child, clinicians should consider underlying causes such as keratoconus, with regular corneal topography recommended.
You can read more about how astigmatism progression in myopia is NOT normal in our article Measuring the whole eye in myopia; and get practical advice in our article Prescribing for the progressing myope with astigmatism.
Anisometropia
Anisometropia, defined as a refractive difference of ≥1.00D between eyes, is a significant amblyopia risk and can impact binocular vision and stereopsis. High anisometropia may indicate underlying ocular pathology which may require co-management with ophthalmology. To date, ortho-k has the strongest evidence for slowing axial elongation in the more myopic eye, with studies showing reduced inter-eye axial length differences over time.
While spectacles can sometimes induce aniseikonia (image size differences) that may impact binocular function, myopia control spectacle lens designs such as the DIMS spectacle lens remain a viable solution for some anisometropic patients—particularly those who are not suitable for, or do not tolerate, contact lenses. These spectacle lenses can provide consistent wear, ease of use, and the ability to incorporate prism or other modifications where needed. Evidence for their use in anisometropia is limited, but they may still offer practical benefits in select cases.
You can read more in our article Monocular Myopia Management: unilateral and anisometropic myopia.
Binocular Vision and Accommodative Disorders: Dual Priorities
Functional vision issues—such as accommodative lag, esophoria, and reduced vergence facility—often co-exist with myopia and may contribute to its progression.
- Prioritising visual comfort: Soojin Nam said that addressing a child’s immediate visual discomfort should always come first. Children with poor accommodative function or latent binocular instability may benefit from vision therapy or base-in prism before, or alongside, myopia control interventions.
- Lens suitability in binocular vision disorders: Bruce Lan noted that MiYOSMART spectacle lenses can generally be prescribed in cases with phoria or accommodative insufficiency, but not in cases of tropia. In strabismic patients, he mentioned concern that misaligned eye may look through the spectacle lens periphery, potentially causing visual blur and discomfort.
- Integrating binocular vision and myopia control: Debbie Jones recommended combining conventional treatments, such as occlusion therapy or vision therapy, with a suitable myopia control strategy. She emphasised that the goal is to preserve or improve binocular function while also limiting myopia progression.
Learn more in our article Four reasons why binocular vision matters in myopia management.
Medical Considerations: Special Populations and Red Flags
Certain medical conditions and syndromes can influence both the safety and suitability of myopia control interventions. These patients often require adapted management strategies, closer monitoring, and collaboration with other healthcare providers.
- Challenges in special populations: Children with developmental delays or disabilities may experience reduced compliance, communication barriers, or difficulty tolerating certain treatments. Spectacles are often the first-line solution due to their ease of use, while contact lenses or atropine may be considered with careful monitoring and strong family support.
- Investigating red flags: Atypical presentations—such as sudden or rapid progression, very high myopia in childhood, or significant changes in astigmatism—should prompt investigation for underlying ocular or systemic pathology. Regular monitoring, appropriate imaging, and timely referral are essential to protect both visual and systemic health.
- Adapting to individual needs: Management plans should be tailored to the child’s medical profile, balancing safety, efficacy, and quality of life. This often requires collaboration between optometry, ophthalmology, and other healthcare professionals to achieve the best outcomes.
We explore how optometry and ophthalmology can and should work together to achieve best outcomes for young myopic patients in our article Collaborative care in myopia management.
Final thoughts
The real-world application of MiYOSMART spectacle lenses demonstrates that myopia management is rarely a one-size-fits-all process. While strong clinical evidence supports their use, patient diversity means that individual factors—ranging from refractive complexity and binocular vision status to co-existing medical conditions—must guide decision-making. By adapting treatment strategies to each child’s needs, integrating multiple interventions when necessary, and maintaining close monitoring, clinicians can optimise both visual outcomes and myopia control efficacy. The experiences shared by these key opinion leaders reinforce that successful management depends on balancing evidence-based practice with the flexibility and creativity required in day-to-day clinical care.
*Case study was shared before range extension of MiYOSMART spectacle lenses. MiYOSMART spectacle lenses are now available up to -13.00D, which benefits not only patients with myopia greater than -10.00D, but is also for patients with myopia less than -10.00D and with astigmatism (e.g. SPH-9.00D/CYL-2.00D)
PRODUCT DISCLAIMER - MiYOSMART has not been approved for myopia management in all countries, including the U.S., and is not currently available for sale in all countries, including the U.S.
The opinions presented are those of the individuals and are not the opinion of HOYA Vision Care or its affiliates or their respective employees. The opinions are presented for informational purposes only and are not intended as medical advice, diagnosis, or choice of treatment. Patients should always consult their Eye Care Professionals for diagnosis and treatment decisions.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented almost 300 conference lectures around the world. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
About Jeanne Saw
Jeanne is a clinical optometrist based in Sydney, Australia. She has worked as a research assistant with leading vision scientists, and has a keen interest in myopia control and professional education.
As Manager, Professional Affairs and Partnerships, Jeanne works closely with Dr Kate Gifford in developing content and strategy across Myopia Profile's platforms, and in working with industry partners. Jeanne also writes for the CLINICAL domain of MyopiaProfile.com, and the My Kids Vision website, our public awareness platform.
This content is brought to you thanks to an educational grant from
References
- Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. Mar 2020;104(3):363-368. [link]
- Leung TW, Lam CSY, Zhang HY, et al. Comparison of myopia progression in individuals wearing defocus incorporated multiple segments (DIMS) spectacle lenses for eight years versus shorter durations. Invest Ophthalmol Vis Sci. Jun 2025;66(8):2820. [link]
- Bullimore MA, Brennan NA. Myopia: An ounce of prevention is worth a pound of cure. Ophthalmic Physiol Opt. Jan 2023;43(1):116-121. [link]
- Xiong S, Sankaridurg P, Naduvilath TJ, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. Sep 2017;95(6):551-566. [link]
- French AN, Ashby RS, Morgan IG, et al. Time outdoors and the prevention of myopia. Exp Eye Res. Sep 2013;114:58-68. [link]
- Flitcroft DI, Harb EN, Wildsoet CF. The Spatial Frequency Content of Urban and Indoor Environments as a Potential Risk Factor for Myopia Development. Invest Ophthalmol Vis Sci. Sep 2020;61(11):42. [link]
Hsin-Yu Yang, Der-Chong Tsai. Efficacy of Defocus Incorporated Multiple Segments (DIMS) Lenses in Retarding Myopic Shifts Among Pre-Myopic Preschoolers: Nine-Month Results of a Pilot Study. Invest. Ophthalmol. Vis. Sci. 2025;66(8):2811.
[link]- Collins MJ, Berntsen DA, Bradley A, et al. IMI - Clinical Myopia Control Trials and Instrumentation Report. Invest Ophthalmol Vis Sci. Feb 2019;60(3):M132-M160. [link]
- Guemes-Villahoz N, Talavero González P, Porras-Ángel P, et al. Atropine and Spectacle lens Combination Treatment (ASPECT): 12-month results of a randomised controlled trial for myopia control using a combination of Defocus Incorporated Multiple Segments (DIMS) lenses and 0.025% atropine. Br J Ophthalmol. Aug 2025;109(9):1074-1080. [link]
- Chung K, Mohidin N, O'Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. Oct 2002;42(22):2555-9. [link]
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci. Aug 2019;96(8):556-567. [link]
- Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci. Oct 2013;54(10):6510-7. [link]
- Chen C, Cho P. Toric orthokeratology for high myopic and astigmatic subjects for myopic control. Clin Exp Optom. Jan 2012;95(1):103-8. [link]
- Tsai HR, Wang JH, Chiu CJ. Effect of orthokeratology on anisometropia control: A meta-analysis. J Formos Med Assoc. Dec 2021;120(12):2120-2127. [link]
- Logan NS, Radhakrishnan H, Cruickshank FE, et al. IMI Accommodation and Binocular Vision in Myopia Development and Progression. Invest Ophthalmol Vis Sci. Apr 2021;62(5):4. [link]
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.












