Clinical
Three clinical pillars for myopia management
In this article:
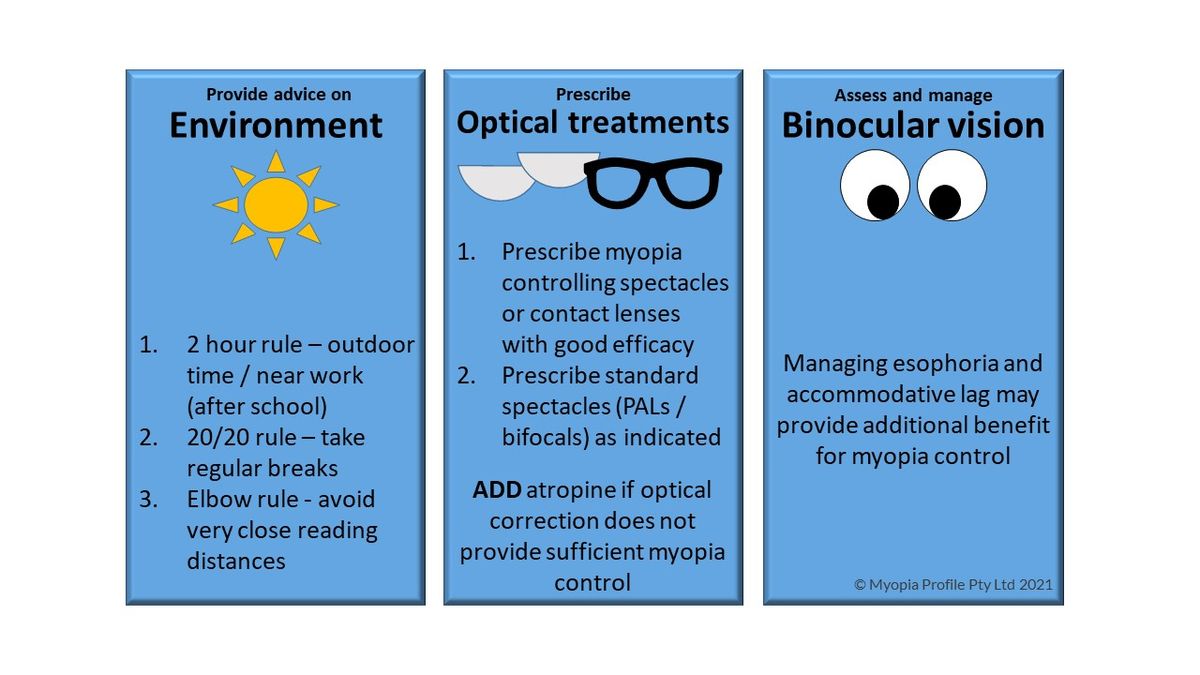
Once the myopia management message has been communicated to the parent and patient - information on expectations, efficacy and safety - and the initial correction has been selected, there are three key areas of clinical focus.
Firstly, advice on visual environment is useful for both the child at risk of myopia development – those with a family history of myopia and less hyperopia than age-normal1 – as well as the myope. Simple advice summarised from the research is provided above, and you can read more on how to explain this in Keys to Communication in Myopia Management.
Secondly, optical treatments should be discussed and offered as first line. The myopic child needs either spectacles or contact lenses for myopia correction, so it makes sense to firstly consider prescribing the best optical treatment available to you, which is suitable for that child and family.
If this is not possible, you can then consider atropine as a first line treatment and/or the next best optical treatments.
So your first prescribing question is spectacles or contact lenses? Along with wide availability of myopia controlling contact lens options, contact lens wear offers numerous functional and psychological benefits to children. Read more Kids And Contact Lenses – Benefits, Safety And Getting To ‘Yes’.
Further reading is available in these clinical articles When to prescribe spectacles for myopia control and When to prescribe atropine for myopia control.
Finally, binocular vision is relevant to myopia management. Since binocular vision disorders such as esophoria and accommodative lag have been implicated in myopia progression,2-6 and also when present provide the greatest efficacy results for progressive spectacle lens myopia management,7, 8 evaluation and management of these issues could provide added benefit to myopia control treatment.
Binocular vision status is additionally relevant to visual comfort – ensuring children have functional skills for reading and schoolwork9, 10 and acceptance of their correction. In time these individual factors may help to predict those who will respond best to particular corrections – for example, OrthoK appears to reduce both esophoria and accommodative lag,11-15 and a Chinese study has shown children with lower accommodative amplitude achieved a 56% better myopia control effect with OK wear over two years.16
In multifocal soft contact lenses, one study linked a reduced accommodative response (increased lag) in the multifocal lens with a reduced myopia control efficacy.17
In future we may be measuring some aspect of accommodation (or several measures) and then selecting a specific contact lens design - maybe smaller zone lenses for normal accommodators and larger zone lenses for underactive accommodators, as indicated by optical modelling.18 For now, including binocular vision factors can bring additional customization to your clinical management decision making, ensuring that visual acuity, visual comfort and visual efficiency are comprehensively addressed for your patient.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
References
- Zadnik K, Sinnott LT, Cotter SA et al (CLEERE Study Group). Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol. 2015;133:683-9. (link)
- Gwiazda J, Bauer J, Thorn F, Held R. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vision Res. 1995;35:1299-304. (link)
- Charman WN. Near vision, lags of accommodation and myopia. Ophthalmic and Physiological Optics. 1999;19:126-33. (link)
- Drobe B, de Saint-André R. The pre-myopic syndrome. Ophthal Physiol Opt. 1995;15:375-8. (link)
- Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82:273-8. (link)
- Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A Ratio, Age, and Refractive Error in Children. Invest Ophthalmol Vis Sci. 2000;41:2469-78. (link)
- Gwiazda J, Hyman L, Hussein M et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492-500. (link)
- Yang Z, Lan W, Ge J et al. The effectiveness of progressive addition lenses on the progression of myopia in Chinese children. Ophthal Physiol Opt. 2009;29:41-8. (link)
- Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Impact of simulated hyperopia on academic-related performance in children. Optom Vis Sci. 2015;92:227-36. (link)
- Quaid P, Simpson T. Association between reading speed, cycloplegic refractive error, and oculomotor function in reading disabled children versus controls. Graefe's Arch Clin Exp Ophthalmol. 2013;251:169-87. (link)
- Gifford KL GP, Hendicott PL, Schmid KL. Binocular visual function in orthokeratology contact lens wear for myopia. Invest Ophthalmol Vis Sci. 2017;58:ARVO E-Abstract 2683878. (link)
- Tarrant J, Liu Y, Wildsoet CF. Orthokeratology Can Decrease the Accommodative Lag in Myopes. Invest Ophthalmol Vis Sci. 2009;50:4294. (link)
- Felipe-Marquez G, Nombela-Palomo M, Palomo-Álvarez C, Cacho I, Nieto-Bona A. Binocular function changes produced in response to overnight orthokeratology. Graefes Arch Clin Exp Ophthalmol. 2017;255:179-88. (link)
- Gifford KL GP, Hendicott PL, Schmid KL. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Cont Lens Anterior Eye. 2017;40:184-9. (link)
- Gifford KL, Gifford P, Hendicott PL, Schmid KL. Zone of Clear Single Binocular Vision in Myopic Orthokeratology. Eye Contact Lens. 2020 Mar;46(2):82-90. (link)
- Zhu M, Feng H, Zhu J, Qu X. The impact of amplitude of accommodation on controlling the development of myopia in orthokeratology. Chinese J Ophthalmol. 2014;50:14-9. (link)
- Cheng X, Xu J, Brennan NA. Accommodation and its role in myopia progression and control with soft contact lenses. Ophthalmic Physiol Opt. 2019 May;39(3):162-171. (link)
- Faria-Ribeiro M, Amorim-de-Sousa A, Gonzalez-Meijome JM. Predicted accommodative response from image quality in young eyes fitted with different dual-focus designs. Ophthalmic Physiol Opt. 2018. (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.











