Clinical
Axial length measurement - a clinical necessity?
In this article:
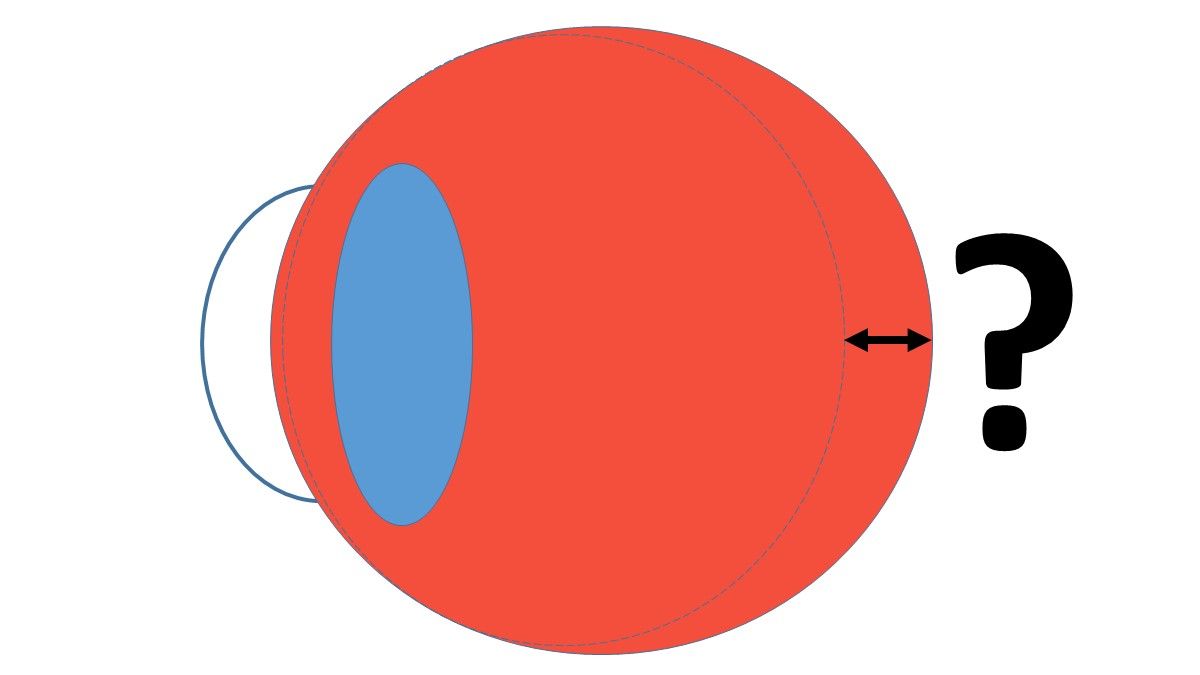
Most eye care practitioners don't routinely measure axial length in clinical practice, mainly due to lack of access to the instrumentation and its expense. This is not the only reason, though, that axial length (AXL) measurement is a bit of a problematic measure for gauging myopia management success in a clinical setting.
When I was leading the authorship of the International Myopia Institute Clinical Management Guidelines, published in February 2019, there was much debate about whether axial length measurement should be written in as a clinical necessity. There is no doubt that it is a necessity for a clinical trial or study of myopia management efficacy – without this data, we simply cannot judge the efficacy of a potential treatment, and how this matches (or mismatches) with refractive control efficacy. However, as a clinical gauge of success axial length measurement is currently a bit problematic. As I wrote during the 2017 International Myopia Conference, Don Mutti and colleagues had analysed the CLEERE data and noted that normal axial elongation during emmetropization is about 0.1mm per year – a bit more for younger children, and a bit less for older children.1 More recently, at the 2018 American Academy of Optometry meeting, Noel Brennan presented the first meta-analysis of axial length which indicated that Asian children show around 40% more axial elongation than Caucasian children,2 which is in line with the meta-analysis of myopic refractive progression published in 2012.3
All of this means that AXL measurement is currently an uncertain diagnostic criteria for the individual myope. In the IMI Clinical Management Guidelines, we settled on including axial length measurement as a 'standard procedure' but with the caveat that there is currently no established criteria for normal or accelerated axial elongation in a given individual.
AXL - absolute and repeated measures
As an absolute measure, I find AXL a useful disease risk indicator for adult myopes, and a useful indicator for urgency of a myopia control strategy in kids, with 26mm being the apparent delineation from the literature.4 If an adult's AXL is over 26mm, I will perform a fundus examination through dilated pupils more regularly, as well as OCT to check the macula. Just recently, I saw a -2.00D, 11 year old with 26.1mm AXL. I'm much more concerned about his progression than the -4.00D 11 year old with 24.5mm AXL.
As a clinical diagnostic factor for repeated measurement, though, things aren't that simple yet. I've been measuring AXL in practice for a few years, but will look at the child's refractive outcomes before explaining these results to parents - I'm simply not sure how to judge the individual's progression based on comparative AXL measures. At this point in time, we don't quite know what constitutes normal or accelerated AXL growth in a child from visit to visit - it appears to depend on age, ethnicity and refractive state. We're starting to get some indication of this from research, but don't yet have the 'growth charts' to make this a reliable diagnostic monitoring measure in practice.
Think of all of the percentile growth charts in children's health management - whether in utero or in childhood, their height and weight by age. In future, I hope we'll have the same for AXL - growth charts of normal emmetropization which take into account age, refractive and ethnicity variations. Early adopter clinicians are already measuring AXL routinely, and a wealth of clinical data will help to inform the establishment of 'norms'. So while currently a little bit complicated as a repeated clinical measure, in a myopia control scientific study there's no doubt that relative measurement of AXL is gold standard and we shouldn't expect anything less.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
References
- Mutti DO. Endpoints in myopia control studies Ophthal Physiol Opt. 2017:Conference proceedings IMC. (link)
- Brennan N, Cheng X, Toubouti Y, Bullimore M. Influence of age and race on axial elongation in myopic children. Optom Vis Sci 2018:Conference proceedings AAO. (link)
- Donovan L, Sankaridurg P, Ho A et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27-32. (link)
- Tideman JW, Snabel MC, Tedja MS et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016;134:1355-63. (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.











